Comprehensive Guide To Breast Cancer Screening And Diagnostic Techniques
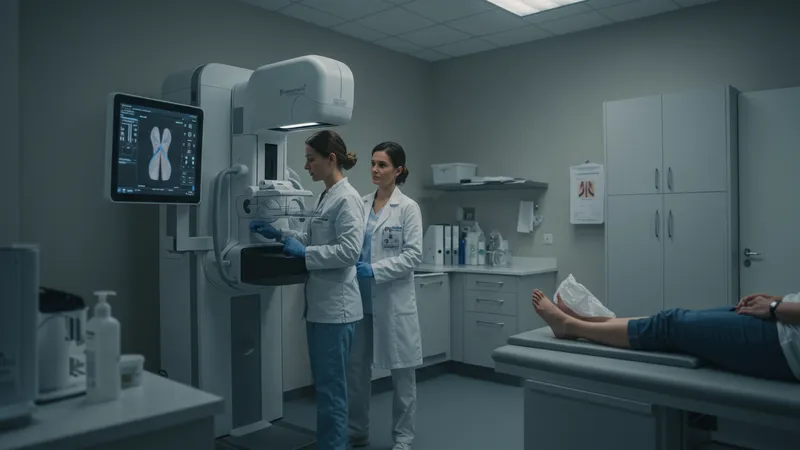
Breast cancer screening and diagnostic techniques are vital for early detection and treatment planning. This comprehensive guide dissects the primary clinical approaches used in the United States to identify, monitor, and diagnose breast cancer, enabling clinicians and patients to make informed decisions. Screening focuses on identifying possible cancer in individuals without symptoms, while diagnostic methods help clarify ambiguous results and determine the exact nature of detected abnormalities.
Understanding these techniques is crucial for American women and healthcare professionals, as regular surveillance can significantly enhance detection rates and potentially impact outcomes. From established imaging tools that lead the field to innovative supplemental technologies, the landscape of breast cancer detection continues to evolve, with improved accuracy and availability.
- Mammography (average cost per screening: $100–$250)
- Breast MRI (average cost per scan: $700–$1,200)
- Ultrasound (average cost per procedure: $100–$400)
- Core Needle Biopsy (average cost: $1,500–$3,000)
- Digital Breast Tomosynthesis (3D Mammography) (average cost per screening: $150–$400)
- Diagnostic Mammography (average procedure cost: $150–$400)
- Stereotactic Biopsy (average cost: $1,000–$2,000)
- PET Scan (average cost: $3,000–$6,000)
- Ductography (average cost: $500–$1,500)
- Fine Needle Aspiration (average cost: $400–$1,000)
Mammography remains the gold standard for population-wide breast cancer screening in the US, recommended annually or biennially for women within certain age brackets. Its accessibility and relatively low cost have propelled it to the forefront of early detection efforts. However, other screening and diagnostic tools, such as breast MRI and ultrasound, offer valuable alternatives and adjuncts, especially for high-risk individuals or those with dense breast tissue.
Digital Breast Tomosynthesis, also known as 3D mammography, is transforming the screening landscape by enhancing the visibility of abnormalities in overlapping tissues. Meanwhile, core needle and stereotactic biopsies allow for accurate tissue sampling when imaging results raise suspicion, both playing a pivotal role in confirming diagnoses without requiring surgical procedures. PET scans contribute to staging and monitoring, particularly in complex or advanced cases, although they are not typically used for primary screening due to their cost and specificity.
Alternative imaging modalities—like ductography—address particular diagnostic challenges, such as abnormal nipple discharge, by visualizing the milk ducts directly. Fine needle aspiration provides a less invasive means to sample suspicious lumps, especially useful in outpatient settings to rule in or out malignancy.
Each technique offers unique advantages, limitations, and appropriate contexts for use. Insurance coverage and regional availability can affect access and affordability in the United States, emphasizing the importance of personalized screening strategies that factor in individual risk profiles, breast density, family history, and physician recommendations.
This comprehensive toolkit underscores the dynamic nature of breast cancer detection and diagnosis in the US. The methods detailed above interconnect, forming an optimized pathway from prevention and early identification to confirmation and staging. The deeper details reveal even more valuable insights ahead, including comparative advantages, innovations, and evolving guidelines that drive effective breast health management.